5 Ways Schizophrenia Affects Military

Introduction to Schizophrenia and Military Service
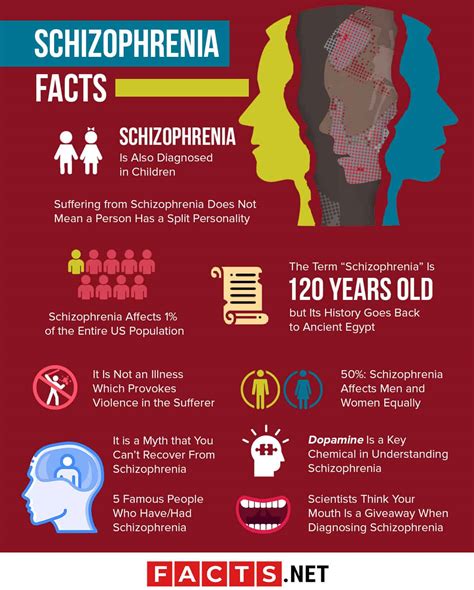
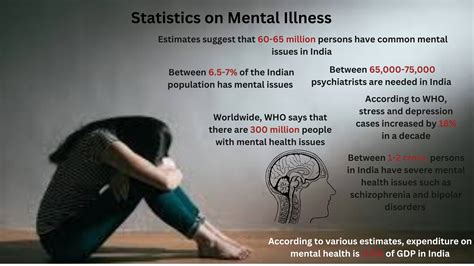
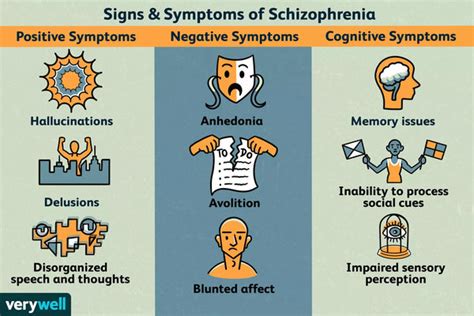
Schizophrenia is a chronic and severe mental disorder that affects how a person thinks, feels, and behaves. It is characterized by distortions in thinking, perception, emotions, language, sense of self, and behavior. Common symptoms of schizophrenia include hallucinations (typically hearing voices), delusions, and severe disordered thinking and behavior that impair daily functioning. For individuals serving in the military, managing such a condition can be particularly challenging due to the high-stress nature of their duties and the importance of cohesion and reliability within military units.
Impact on Military Performance
Military service requires individuals to be in top physical and mental condition. Schizophrenia can significantly affect an individual’s ability to perform their military duties. The symptoms of schizophrenia can lead to difficulties in following commands, making sound judgments, and interacting appropriately with colleagues. This can compromise not only the individual’s safety but also the safety and effectiveness of their team. Furthermore, the unpredictable nature of schizophrenia symptoms can make it challenging for commanders to assign tasks and missions, knowing that the individual’s condition could deteriorate at any moment.
Diagnosis and Treatment Challenges

Diagnosing and treating schizophrenia in the military can be more complicated than in the civilian population. Military personnel often face unique stressors, such as deployment, combat, and frequent moves, which can exacerbate symptoms of schizophrenia or complicate its diagnosis. Moreover, the stigma associated with mental health issues can discourage military personnel from seeking help, fearing it might affect their career. Early intervention is crucial in managing schizophrenia, and thus, creating an environment where military personnel feel comfortable seeking medical help without fear of repercussions is essential.
Social and Relational Challenges
Living with schizophrenia can be isolating, and for military personnel, this isolation can be even more pronounced. The nature of military life, with its emphasis on camaraderie and unit cohesion, can make it difficult for individuals with schizophrenia to connect with their peers or form meaningful relationships. Furthermore, the symptoms of schizophrenia, such as social withdrawal or unusual behavior, can lead to misunderstandings or fears among fellow soldiers, further exacerbating feelings of loneliness and isolation. Support systems, including understanding commanders, peers, and access to mental health professionals, are vital in helping military personnel with schizophrenia navigate these challenges.
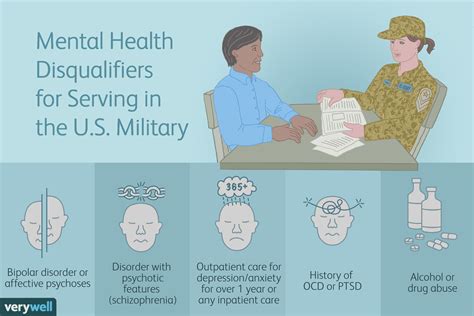
Security Clearances and Career Implications

For military personnel, especially those in roles requiring security clearances, having a mental health condition like schizophrenia can have significant career implications. The process of obtaining or maintaining a security clearance involves a thorough evaluation of an individual’s mental health, among other factors. Disclosing a schizophrenia diagnosis can lead to the denial or revocation of a security clearance, which in turn can limit career advancement opportunities or even lead to discharge from the military. This adds another layer of complexity for military personnel dealing with schizophrenia, as they must balance the need for treatment and honesty about their condition with the potential professional consequences.
Support and Accommodation
Despite the challenges, there are ways to support military personnel with schizophrenia. Accommodations can be made to help individuals manage their condition effectively while continuing to serve. This might include adjustments to their duties, flexible scheduling to accommodate therapy sessions, or providing access to mental health resources and support groups. Additionally, educating military commanders and personnel about schizophrenia can help reduce stigma and promote a more supportive environment. It’s also important for military mental health services to be equipped to provide specialized care for schizophrenia, including medication management and psychotherapy tailored to the unique needs and circumstances of military life.
👥 Note: Creating a supportive and understanding environment within military units is crucial for helping personnel with schizophrenia manage their condition and fulfill their duties effectively.
In essence, schizophrenia presents a complex set of challenges for military personnel, affecting their performance, relationships, and career prospects. However, with the right support, accommodations, and understanding, it is possible for individuals with schizophrenia to serve effectively and manage their condition. The key lies in fostering an open and supportive military culture that encourages seeking help without fear of judgment or repercussions, alongside providing accessible and specialized mental health services.
How does schizophrenia affect military personnel differently than the general population?
+
Schizophrenia can affect military personnel differently due to the unique stressors of military life, such as combat, deployment, and the need for cohesion and reliability within units. These factors can exacerbate symptoms and complicate diagnosis and treatment.
Can military personnel with schizophrenia continue to serve?
+
Yes, with the right treatment and support, military personnel with schizophrenia can continue to serve. However, their ability to perform certain duties may be limited, and accommodations may be necessary to ensure their safety and the safety of others.
How can military culture support personnel with schizophrenia?

+
Military culture can support personnel with schizophrenia by promoting openness about mental health issues, reducing stigma, and providing accessible mental health services. Education about schizophrenia and its effects can also help commanders and peers understand and support affected individuals.



